Basal Cell Carcinoma and its Impact

Regarding skin cancer, basal cell carcinoma (BCC) is the most common type. It affects millions worldwide and has become a growing concern in recent years. Understanding the causes, symptoms, diagnosis, and treatment options for basal cell carcinoma is crucial for individuals seeking reliable information.
What is Basal Cell Carcinoma?
Basal cell carcinoma is a type of skin cancer originating in the basal cells responsible for producing new skin cells. These cells are found in the epidermis’s deepest layer, the skin’s outermost layer. Although basal cell carcinoma rarely spreads to other body parts, it can cause significant damage if left untreated.
Causes of Basal Cell Carcinoma
Overview of Skin and its Layers
To understand the causes of basal cell carcinoma, it is important to have a basic understanding of the skin and its layers. The skin is the largest organ of the body. It consists of three primary layers: the epidermis, the dermis, and the subcutaneous tissue.
UV Radiation and its Role in Causing Basal Cell Carcinoma
One of the leading causes of basal cell carcinoma is exposure to ultraviolet (UV) radiation from the sun or artificial sources, such as tanning beds. Prolonged and unprotected exposure to UV radiation can damage the DNA in skin cells, leading to the development of cancerous cells.
Other Risk Factors Associated with Basal Cell Carcinoma
While UV radiation is the primary cause, several other risk factors increase the likelihood of developing basal cell carcinoma. These factors include:
- Fair Skin and Light Hair: Individuals with fair skin, light hair, and light-colored eyes are at higher risk due to reduced melanin, which provides natural protection against UV radiation.
- Chronic Exposure to Sunlight: People with occupations or hobbies that involve prolonged exposure to sunlight are more susceptible to basal cell carcinoma.
- Family History and Genetic Factors: A family history of skin cancer, particularly basal cell carcinoma, increases the risk of developing the disease. Certain genetic conditions also contribute to the development of basal cell carcinoma.
- Weakened Immune System: Individuals with weakened immune systems, such as those undergoing organ transplants or diagnosed with immunosuppressive disorders, are more prone to basal cell carcinoma.
Preventive Measures and Sun Protection
Adopting sun protection measures to reduce the risk of basal cell carcinoma is crucial. These include:
- Applying sunscreen with a high SPF regularly
- Wearing protective clothing and wide-brimmed hats
- Seeking shade during peak sun hours
- Avoiding tanning beds and artificial sources of UV radiation
Early Signs and Symptoms of Basal Cell Carcinoma
Basal cell carcinoma often presents with visible symptoms that should not be ignored. Some common signs to watch out for include:
- Persistent Open Sores or Lesions: Non-healing sores or lesions that may crust, bleed, or ooze are a common early indication of basal cell carcinoma.
- Shiny or Pearly Bumps with a Translucent Appearance: Raised, shiny, and pearly bumps that may have visible blood vessels are often seen in basal cell carcinoma.
- Pink Growths with Raised Edges: Pink, red, or white growths with raised edges and a central indentation are another characteristic symptom.
- Scaly Patches or Red Patches: Flat, scaly, or reddish patches on the skin that may itch or cause discomfort can indicate basal cell carcinoma.
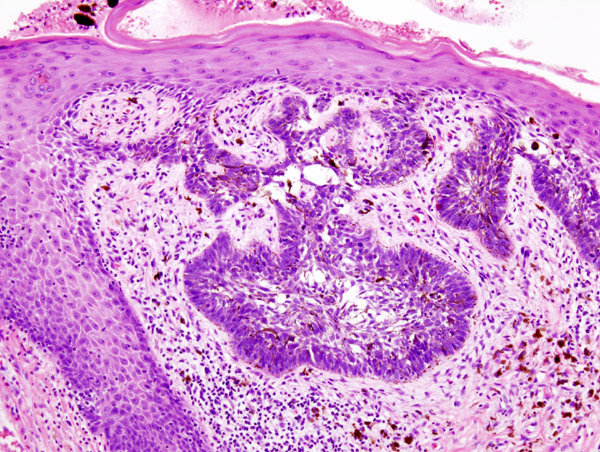
Understanding the Different Subtypes of Basal Cell Carcinoma
Basal cell carcinoma can manifest in different subtypes, each with unique characteristics. Understanding these subtypes can help in identifying and diagnosing the condition accurately. The main subtypes of basal cell carcinoma include:
- Nodular Basal Cell Carcinoma: This is the most common subtype and typically appears as a flesh-colored or pink nodule with a smooth, shiny surface. It may also have visible blood vessels and can ulcerate or form a crust.
- Superficial Basal Cell Carcinoma: This subtype often presents as a red, scaly, or slightly raised patch on the skin. It may resemble a persistent rash or eczema on the trunk and extremities.
- Pigmented Basal Cell Carcinoma: Pigmented basal cell carcinoma is characterized by brown or black pigmentation within the lesion. It can be mistaken for a benign mole or melanoma, highlighting the importance of proper diagnosis.
- Morpheaform Basal Cell Carcinoma: Morpheaform or sclerosing basal cell carcinoma is a less common but more aggressive subtype. It appears as a firm, pale, scar-like plaque with indistinct borders. Morpheaform basal cell carcinoma can be challenging to diagnose and treat due to its infiltrative nature.
It’s worth noting that some cases may exhibit features of multiple subtypes, making diagnosis more complex. Therefore, seeking medical attention for a proper diagnosis and timely treatment is crucial if you notice any suspicious skin changes or symptoms.
Diagnosis of Basal Cell Carcinoma
Diagnosing basal cell carcinoma involves a combination of physical examination, medical history assessment, and, in some cases, additional tests. The diagnostic process may include:
Physical Examination and Medical History Assessment
A dermatologist will thoroughly examine the skin during a physical examination, paying particular attention to any suspicious areas or lesions. They will also inquire about your medical history, including any family history of skin cancer or previous sun exposure.
Biopsy and Laboratory Tests
A biopsy will confirm the diagnosis if a suspicious lesion is identified. A small tissue sample is taken from the affected area and sent to a laboratory for microscopic examination. The biopsy results will determine whether the lesion is cancerous and the specific subtype of basal cell carcinoma.
Imaging Tests and Advanced Diagnostic Techniques
In some cases, imaging tests and advanced diagnostic techniques may be used to aid in the diagnosis of basal cell carcinoma. These include:
- Dermoscopy: Dermoscopy is a non-invasive technique that allows dermatologists to examine skin lesions using a specialized handheld device. It provides a magnified view of the skin and helps identify specific features indicative of basal cell carcinoma.
- Confocal Microscopy: Confocal microscopy is a high-resolution imaging technique that enables skin examination at a cellular level. It can help differentiate between cancerous and non-cancerous cells, aiding in accurate diagnosis.
- Reflectance Confocal Microscopy: Reflectance confocal microscopy is a newer imaging technique that provides real-time images of the skin at a cellular level. It allows for precise visualization of individual skin layers and can assist in determining the extent of basal cell carcinoma.
These advanced diagnostic techniques can be particularly helpful in cases where the diagnosis is challenging or when determining the extent of the cancerous growth.
It is important to emphasize that only a qualified healthcare professional can accurately diagnose basal cell carcinoma. Therefore, if you notice any suspicious skin changes or symptoms, it is crucial to consult a dermatologist for a comprehensive evaluation.
Treatment Options for Basal Cell Carcinoma
The treatment approach for basal cell carcinoma depends on various factors, including the size, location, subtype, and extent of the cancerous growth and the individual’s overall health. Treatment goals typically include completely removing cancer while preserving function and achieving an optimal cosmetic outcome. Several treatment options are available, ranging from non-surgical methods to surgical interventions and emerging therapies:
Non-Surgical Treatment Options
- Topical Medications and Creams: Topical medications such as imiquimod or 5-fluorouracil may be prescribed for superficial or small basal cell carcinomas. These creams stimulate the body’s immune response to target and eliminate cancer cells.
- Photodynamic Therapy (PDT): PDT involves applying a light-sensitive medication to the affected area, followed by exposure to a specific wavelength of light. The medication selectively targets and destroys cancer cells when activated by light while minimizing damage to healthy tissue.
Surgical Treatment Options
- Excisional Surgery: Excisional surgery removes the cancerous lesion and a surrounding margin of healthy tissue. The excised tissue is then examined under a microscope to ensure complete removal of the cancer cells. This method is commonly used for most types and sizes of basal cell carcinomas.
- Mohs Surgery: Mohs surgery is a specialized surgical technique used for treating complex or recurrent basal cell carcinomas, as well as those located in areas where tissue preservation is critical (e.g., face, ears). It involves removing the tumor layer by layer, with each layer examined microscopically, ensuring complete removal while sparing healthy tissue.
- Curettage and Electrodesiccation: This technique involves scraping off the cancerous growth using a curette (a spoon-shaped instrument) and then searing the area with an electric needle to control bleeding and destroy the remaining cancer cells. It is commonly used for small, superficial basal cell carcinomas.
Other Emerging Treatment Modalities
- Cryosurgery: Cryosurgery involves freezing cancer cells using liquid nitrogen, which destroys them. It is suitable for small, superficial basal cell carcinomas and can be performed in an outpatient setting.
- Radiation Therapy: In cases where surgery is not feasible or appropriate, radiation therapy may be employed. High-energy X-rays are directed at the tumor, damaging cancer cells and preventing their growth. Radiation therapy is often used for larger or invasive basal cell carcinomas or individuals who are not surgical candidates.
- Laser Therapy: Laser therapy uses intense, focused light to destroy cancer cells. It can be effective for superficial basal cell carcinomas and offers precise targeting while minimizing damage to surrounding healthy tissue.
- Immunotherapy and Targeted Therapy: Advanced cases of basal cell carcinoma or those resistant to conventional treatments may benefit from immunotherapy or targeted therapy. These therapies utilize drugs that target specific cellular mechanisms or boost the body’s immune system to fight cancer cells.
Factors Influencing Treatment Choice
Treatment choice depends on various factors, including basal cell carcinoma’s size, location, and subtype and the individual’s overall health and personal preferences. In addition, factors such as the potential for scarring, cosmetic outcome, and functional considerations also play a role in determining the most appropriate treatment approach. Therefore, it is crucial to have a detailed discussion with a dermatologist or a specialist to determine the best course of treatment for each individual case.
Recovery and Follow-Up Care
Following treatment for basal cell carcinoma, proper recovery and diligent follow-up care are essential to ensure optimal healing and monitor for any signs of recurrence. Here are some important aspects to consider:
Post-Treatment Care Guidelines
After surgical interventions or other treatments, healthcare providers will provide specific post-treatment care instructions. These guidelines may include:
- Wound Care: Proper wound care is crucial to promote healing and reduce the risk of infection. It may involve keeping the treated area clean, applying topical medications or dressings as instructed, and avoiding activities that could disrupt the healing process.
- Pain Management: Depending on the treatment method, discomfort or pain may be experienced. Healthcare providers may recommend over-the-counter pain relievers or prescription medications to manage pain during recovery.
- Activity Restrictions: Depending on the location and extent of the treatment, temporary activity restrictions may be advised. This could involve avoiding strenuous activities, excessive sun exposure, or certain movements that could strain the treated area.
Healing Process and Potential Side Effects
The healing process for basal cell carcinoma treatment varies depending on the specific treatment method and individual factors. However, some common aspects of the healing process include:
- Scarring: Surgical interventions may leave scars, but the extent and visibility of scars can vary. Mohs surgery aims to preserve healthy tissue and minimize scarring, while other surgical methods may result in more noticeable scars. Proper wound care during the healing process can help optimize the cosmetic outcome.
- Redness and Swelling: It is common to experience temporary redness, swelling, and mild bruising in the treated area. These side effects typically subside over time, but following the recommended care guidelines and seeking medical advice if they persist or worsen is important.
- Changes in Sensation: In some cases, there may be temporary or permanent changes in sensation, such as numbness, tingling, or sensitivity, in the treated area. This can occur due to nerve involvement during surgery or as a result of tissue healing.
- Follow-Up Monitoring: Regular follow-up visits with healthcare providers are crucial to monitor the healing process and check for any signs of recurrence or complications. These appointments may include physical examinations, imaging tests, or other diagnostic procedures as deemed necessary.
Importance of Regular Follow-Up Visits and Monitoring
Even after successful treatment, individuals with basal cell carcinoma should maintain regular follow-up visits with healthcare providers. These visits serve several purposes:
- Surveillance for Recurrence: Basal cell carcinoma has a chance of recurrence, particularly in individuals who have had it. Regular monitoring allows healthcare providers to detect any signs of a recurrence early when treatment is most effective.
- Skin Examination: Routine skin examinations enable healthcare providers to identify new or suspicious lesions that may require further evaluation. This is especially important for individuals with a history of basal cell carcinoma or other forms of skin cancer.
- Education and Prevention: Follow-up visits allow healthcare providers to educate individuals about sun protection measures, early detection, and prevention strategies. They can offer guidance on lifestyle changes and skin self-examination and raise awareness about the importance of regular skin checks.
By attending regular follow-up visits and adhering to the recommended monitoring schedule, individuals can proactively manage their skin health and ensure early detection and prompt treatment of potential issues.
Prevention and Risk Reduction Strategies
While basal cell carcinoma is a common form of skin cancer, several preventive measures can help reduce the risk of developing this condition. By adopting sun protection strategies and lifestyle changes, individuals can minimize exposure to harmful UV radiation and protect their skin. Here are some effective prevention and risk-reduction strategies:
Sun Protection Measures and Lifestyle Changes
- Use Sunscreen: Apply a broad-spectrum sunscreen with a high SPF (Sun Protection Factor) of 30 or higher on all exposed skin areas, even on cloudy days. Reapply sunscreen every two hours or more frequently if sweating or swimming.
- Seek Shade: Limit direct exposure to the sun during peak hours, typically between 10 a.m. and 4 p.m. Seek shade under trees and umbrellas or wear protective clothing outdoors.
- Wear Protective Clothing: Opt for loose-fitting, tightly woven clothing that covers the arms, legs, and body. Use wide-brimmed hats to shade the face, neck, and ears. Consider wearing UV-protective sunglasses to shield the eyes from harmful UV radiation.
- Avoid Tanning Beds and Artificial UV Radiation Sources: Tanning beds and sunlamps emit harmful UV radiation and increase the risk of skin cancer. It is best to avoid using them altogether.
Self-Examination and Early Detection
- Perform Regular Skin Self-Examinations: Conduct regular self-examinations of your skin to identify any new or changing moles, spots, or lesions. Use a mirror to check hard-to-see areas or ask a partner for assistance.
- Follow the ABCDE Rule: When examining moles or suspicious spots, follow the ABCDE rule:
A: Asymmetry – Check if one half of the mole or spot differs from the other half.
B: Border – Look for irregular, uneven, or poorly defined borders.
C: Color – Observe for variations in color or the presence of multiple colors within the same mole or spot.
D: Diameter – Take note of any growth larger than the size of a pencil eraser (usually 6 mm).
E: Evolution – Pay attention to changes in size, shape, color, or symptoms of itching, bleeding, or crusting. - Seek Professional Evaluation: If you notice any concerning changes in your skin or suspicious lesions, seek professional evaluation from a dermatologist or healthcare provider. Early detection and timely treatment can significantly improve outcomes.
Genetic Counseling and Screening for High-Risk Individuals
- Family History Assessment: If there is a family history of skin cancer, particularly basal cell carcinoma, consider discussing this with a healthcare provider. They may recommend genetic counseling and screening for individuals with a higher risk due to genetic predisposition.
- Genetic Counseling: Genetic counseling can help individuals understand their genetic risk factors for developing basal cell carcinoma. It involves thoroughly evaluating family history and personalized guidance on risk management and preventive measures.
Public Awareness Campaigns and Education
- Stay Informed: Keep yourself updated on the latest information about skin cancer, including basal cell carcinoma. Reliable sources such as medical journals, reputable websites, and healthcare professionals can provide valuable insights and resources.
- Participate in Public Awareness Campaigns: Support and engage in public awareness campaigns that promote sun safety, skin cancer prevention, and early detection. Share educational materials, participate in community events, and encourage others to prioritize their skin health.
By adopting these preventive measures and promoting skin health awareness, individuals can reduce their risk of developing basal cell carcinoma and other forms of skin cancer.
The Psychological and Emotional Impact of Basal Cell Carcinoma
Dealing with a diagnosis of basal cell carcinoma can significantly impact individuals psychologically and emotionally. Understanding and addressing these aspects of the journey are crucial for overall well-being. Here are some key considerations:
Coping with a Diagnosis and Treatment Journey
- Emotional Responses: It is normal to experience a range of emotions upon receiving a diagnosis of basal cell carcinoma. Feelings of fear, anxiety, sadness, anger, or frustration may arise. Recognize and acknowledge these emotions, and don’t hesitate to seek support from loved ones, support groups, or mental health professionals.
- Information and Education: Educate yourself about basal cell carcinoma to better understand the condition, treatment options, and prognosis. Reliable sources, such as medical professionals or reputable organizations, can provide accurate and helpful information.
- Open Communication: Maintain open and honest communication with your healthcare team. Ask questions, share concerns, and express any emotional or psychological challenges you may face. They can provide guidance and support and connect you with additional resources.
Support Networks and Resources for Emotional Well-Being
- Seek Support: Lean on your support network, including family, friends, and loved ones. Discuss your feelings, concerns, and experiences with them. Their understanding and empathy can provide emotional comfort and a sense of connectedness.
- Support Groups: Consider joining support groups for individuals with skin cancer or specifically for basal cell carcinoma. These groups provide a platform to share experiences, receive support, and learn coping strategies from others who have gone through similar journeys.
- Professional Counseling: If the emotional impact overwhelms or interferes with daily life, consider seeking professional counseling or therapy. Mental health professionals can offer specialized guidance and support to help navigate the emotional challenges associated with basal cell carcinoma.
- Psychological Support Services: Many healthcare facilities have psychological support services specifically tailored to cancer patients. These services may include counseling, therapy, stress management techniques, and resources for emotional well-being.
- Self-Care and Stress Management: Engage in self-care practices promoting relaxation and reducing stress. This may include meditation, deep breathing exercises, mindfulness, hobbies, or engaging in activities that bring joy and peace of mind.
Remember that taking care of your emotional well-being is as important as physical treatment. Therefore, seeking help and support during this challenging time is okay.
Conclusion
Basal cell carcinoma, a common skin cancer, requires understanding and proactive management. Practicing sun protection, recognizing symptoms, seeking an early diagnosis, and exploring treatment options are key.
UV radiation is a significant cause of basal cell carcinoma, highlighting the importance of sun-safe behaviors. Regular use of sunscreen, seeking shade, and avoiding tanning beds reduce the risk of developing this skin cancer.
Understanding treatment options is crucial upon diagnosis. Non-surgical approaches like topical medications and photodynamic therapy may suffice. At the same time, surgical interventions such as excisional or Mohs surgery may be necessary.
Emerging therapies like cryosurgery, radiation, lasers, immunotherapy, and targeted treatments provide additional options.
Recovery and follow-up care play vital roles. Adhering to post-treatment guidelines, monitoring healing, and attending regular check-ups ensure proper recovery and early detection of potential recurrence.
Prevention strategies are paramount. Adopting sun protection, self-examination, and genetic counseling for high-risk individuals lowers the chances of basal cell carcinoma.
Addressing the psychological impact is essential. Coping with emotions, seeking support from loved ones and groups, and considering professional counseling help individuals navigate the challenges associated with this condition.
In conclusion, early detection, prompt treatment, and ongoing vigilance are key in managing basal cell carcinoma. In addition, prioritizing sun safety, staying informed, and adopting preventive measures empower individuals to effectively manage this skin cancer and maintain overall well-being.
FAQs
Is basal cell carcinoma a serious form of skin cancer?
While basal cell carcinoma rarely spreads to other body parts, it can cause significant damage if left untreated. Early detection and treatment are crucial for successful management.
Can basal cell carcinoma be prevented entirely?
While preventing basal cell carcinoma entirely may be impossible, adopting sun protection measures and avoiding excessive UV radiation exposure can significantly reduce the risk.
Are there any long-term side effects of basal cell carcinoma treatment?
The long-term side effects of treatment depend on the specific method used and individual factors. Some treatments may result in scarring, changes in sensation, or cosmetic alterations. Discuss potential side effects with your healthcare provider before treatment.
Is basal cell carcinoma hereditary?
While there is a genetic component to basal cell carcinoma, it is not solely hereditary. Family history can increase the risk, but factors like sun exposure and individual susceptibility also play a role.
Can basal cell carcinoma recur after treatment?
Although treatment aims to remove the cancer completely, there is a chance of recurrence. Regular follow-up visits with healthcare providers are essential to monitor for any signs of recurrence and ensure early intervention.