For many, Dermatitis Herpetiformis (DH) may not ring a bell. Yet, for the individuals grappling with this persistent skin condition, it’s an everyday battle that profoundly influences their quality of life. Often designated as the ‘celiac disease of the skin,’ Dermatitis Herpetiformis is a persistent skin condition presenting as intensely itchy blisters and skin rashes.

Unraveling the Causes and Risk Factors of Dermatitis Herpetiformis
Dermatitis Herpetiformis’s interplay of causes and risk factors is akin to a sophisticated dance. It’s a complex choreography of genetic, environmental, and immune elements that result in this unique skin manifestation.
To truly comprehend Dermatitis Herpetiformis, we must first acknowledge its close relationship with celiac disease. I like to think of them as two sides of the same coin. Celiac disease affects the gut, while DH expresses itself on the skin. Still, both are rooted in the same gluten-induced autoimmune response.
Genetics plays a significant role in this equation. Certain genetic markers, specifically HLA-DQ2 and HLA-DQ8, are often present in those with Dermatitis Herpetiformis. However, these markers alone do not dictate the development of DH, indicating the presence of other contributing factors.
Environmental triggers, particularly ingesting gluten, can set off this autoimmune response in susceptible individuals. When someone with Dermatitis Herpetiformis consumes gluten, their immune system reacts abnormally, deposing IgA antibodies in the skin and causing DH’s characteristic itchy, blistering rash.
It’s crucial to remember that Dermatitis Herpetiformis is not a result of poor hygiene or contagious infection. It’s an autoimmune skin condition intrinsically linked with celiac disease and gluten sensitivity. Understanding the causes and risk factors can pave the way to effective management strategies and, in the future, prevention.

Diagnosing Dermatitis Herpetiformis: Piecing Together the Puzzle
The diagnosis of Dermatitis Herpetiformis, much like the disease itself, is a bit of a puzzle. It’s a process that requires a keen eye, a systematic approach, and a comprehensive understanding of the disease. As an immunologist, I am no stranger to this intricate process, and in this section, I’ll guide you through it step by step.
Symptoms: The First Piece of the Puzzle
DH is primarily characterized by an intensely itchy rash and blisters. These usually appear on the elbows, knees, buttocks, back, or scalp. However, these symptoms alone are not enough for a diagnosis. They could indicate several skin conditions, and it’s essential to rule these out.
Patient’s History: The Second Piece of the Puzzle
This is where the second piece of the puzzle comes into play – the patient’s history. Doctors will often ask about the patient’s diet, family history, and any associated gastrointestinal symptoms. This information can provide vital clues and direct the diagnostic process.
Testing: The Third Piece of the Puzzle
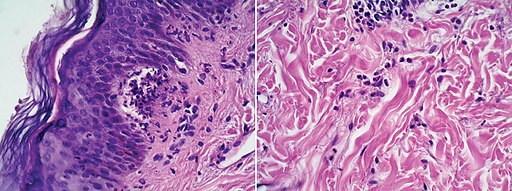
The third piece of the puzzle is testing. A skin biopsy is usually performed to confirm the diagnosis. During this procedure, a small skin sample is taken from the area next to a blister and examined under a microscope. In DH, the skin sample will typically show clusters of a certain type of immune cell called neutrophils.
Blood Test: Yet Another Piece of the Puzzle
Yet another piece of the puzzle is the blood test. Doctors often test for certain antibodies in the blood that are commonly found in people with DH. These include IgA endomysial antibodies and IgA tissue transglutaminase antibodies.
The Final Picture
Once all these puzzle pieces are put together, a clear picture of DH can emerge. However, it’s important to remember that every patient is unique, and the puzzle of DH may only sometimes be straightforward. There can be variations, exceptions, and even false positives or negatives. Therefore, an experienced healthcare provider’s insight is crucial in correctly diagnosing this complex condition.

Treatment Options for Dermatitis Herpetiformis: A Route to Relief
Addressing Dermatitis Herpetiformis isn’t a one-size-fits-all endeavor. Treatment is multifaceted, personalized, and, at times, complex. As an immunologist, I can attest that finding the right treatment requires scientific knowledge, patient insight, and clinical expertise. Let’s walk through the primary treatment options for DH.
The cornerstone of DH treatment is a strict, lifelong gluten-free diet. While this might sound daunting, it’s important to remember that this dietary adjustment has the power to alleviate skin symptoms and any associated intestinal damage. It’s about more than just avoiding bread and pasta. Gluten can be found in many products, from salad dressings to lip balms, so it’s essential to become a careful and conscious consumer.
Medications also play a critical role in managing DH. Dapsone, an antibiotic, is commonly used to alleviate itching and clear skin lesions. This medication acts quickly, often providing relief within days. However, Dapsone doesn’t address the underlying cause of the disease; it only eases the symptoms. This is why it’s often used in conjunction with a gluten-free diet.
Doctors may sometimes prescribe other medications, such as sulfapyridine or immunosuppressants, particularly if the patient cannot tolerate Dapsone. These drugs can also help control symptoms but come with their own set of potential side effects.
It’s important to note that while these treatments can help manage the symptoms of DH, they don’t cure the disease. DH is a chronic condition, and managing it is a long-term commitment. But with the right treatment plan, patients can lead a symptom-free life.
Living with Dermatitis Herpetiformis: Navigating the Challenges
Living with Dermatitis Herpetiformis is about more than just managing symptoms and following a treatment plan. It’s about learning to navigate the daily challenges of a chronic skin condition.
One of the key challenges is maintaining a strict gluten-free diet. It’s about more than avoiding bread, pasta, and other obvious sources of gluten. Gluten can be hidden in everyday products, from sauces and seasonings to medications and cosmetics. Identifying and avoiding these hidden sources of gluten is a vital part of managing DH.
Another challenge is dealing with the itch. DH is known for causing an intense, persistent itch that can interfere with sleep, work, and daily activities. Over-the-counter treatments and home remedies, such as cool compresses or oatmeal baths, can provide some relief. However, effective itch management often involves lifestyle changes, medication, and coping strategies for many people.
Perhaps one of the less talked about but equally significant challenges of living with DH is the emotional toll it can take. The constant vigilance required to avoid gluten, the struggle with itching and discomfort, and the impact on appearance can all contribute to feelings of anxiety, frustration, and low self-esteem. It’s important to acknowledge these feelings and seek support when needed, whether from a mental health professional, a support group, or loved ones.
Dermatitis Herpetiformis in Different Demographics
Dermatitis Herpetiformis doesn’t discriminate. It can affect people of all ages and genders, but its impact can vary depending on these factors.
A. Children and Dermatitis Herpetiformis
While Dermatitis Herpetiformis is more commonly diagnosed in adults, children can also be affected. The impact on children can be significant, given the itchy, uncomfortable rash and the need for dietary restrictions. Children with Dermatitis Herpetiformis often require additional support at school and home to manage their condition effectively.
B. Dermatitis Herpetiformis in Adults
Dermatitis Herpetiformis typically appears in adults in their 20s or 30s, but it can develop at any age. Maintaining a strict gluten-free diet can pose challenges in social situations and require significant lifestyle changes.
C. Gender Differences
Research suggests that men are slightly more likely to develop Dermatitis Herpetiformis than women. However, both genders face the same challenges when managing the condition.
Understanding these differences can help tailor the management and treatment of Dermatitis Herpetiformis to meet the specific needs of different demographic groups.
The Impact of Dermatitis Herpetiformis on Daily Life: A Closer Look
Understanding the impact of Dermatitis Herpetiformis on daily life involves peeling back the layers of this complex condition. As a healthcare professional, I’ve observed that while the physical symptoms of DH are often the most noticeable, the disease’s effects can ripple out, affecting various aspects of a person’s life.
The physical impact of DH is clear. The persistent itch, the discomfort of blisters, and the need for constant skin care can be taxing. Everyday tasks can become challenging, and the discomfort may disrupt activities such as exercise or sleep.
Beyond the physical, the dietary restrictions associated with DH can also take a toll. Maintaining a strict gluten-free diet can be challenging and time-consuming. It requires careful planning and preparation, especially when dining out or traveling. Moreover, there may be a feeling of loss or frustration over avoiding favorite foods or cuisines.
But perhaps the most under-recognized impact of DH is the emotional and psychological burden it can carry. The chronic nature of the disease, the ongoing management, and the visible symptoms can lead to stress, anxiety, and even depression. It’s not uncommon for people with DH to feel isolated or misunderstood due to their condition.
Living with DH is undoubtedly challenging, but it’s important to remember that help is available. Medical treatments, dietary guidance, and psychological support can improve the quality of life for those with DH.
The Latest Research and Advances: Towards a Future Free of Dermatitis Herpetiformis
The realm of Dermatitis Herpetiformis research is as dynamic and intricate as the disease itself.
One of the most promising research areas is exploring new treatment options. Scientists are investigating other anti-inflammatory and immunosuppressive drugs that could potentially offer relief for those with DH. For instance, studies are underway to evaluate the efficacy of drugs like methotrexate and cyclosporine, which have shown promise in other autoimmune conditions.
Additionally, scientists are delving deeper into the genetic aspects of DH. By understanding the genetic factors contributing to the disease, researchers hope to develop targeted therapies to treat DH at its source rather than just managing its symptoms. This could revolutionize how we approach DH treatment in the future.
The gluten-free diet, the cornerstone of DH management, is also an area of ongoing research. Scientists are looking at ways to make the diet more manageable and less restrictive. This includes investigating potential treatments that could allow people with DH to tolerate small amounts of gluten without triggering symptoms.
In DH research, there is a constant push towards a future where DH can be more effectively managed or perhaps even cured. While there is still much to learn, these advancements offer hope for those with the condition.
Nutrition and Diet
The arena of nutrition plays an integral role in managing Dermatitis Herpetiformis. It’s more than just about keeping the rashes at bay; it’s about a lifestyle pivot towards a gluten-free diet. This involves keenly inspecting food labels, learning about hidden sources of gluten, and making informed dietary choices.
Dermatitis Herpetiformis: Navigating a New Normal
Understanding Dermatitis Herpetiformis is the first step toward navigating a new normal. As I researched, it has shown me that while DH is a lifelong condition, it can also be managed effectively with the right approach.
The most important aspect of this approach is adherence to a strict gluten-free diet. While it may seem daunting at first, many people find that with time and practice, they can adapt to this new way of eating and even discover new favorite foods.
Another key part of living with DH is managing the itch. There are various methods available, from over-the-counter creams to prescription medications. It’s about finding what works best for you and incorporating it into your daily routine.
Finally, living with DH also means taking care of your emotional well-being. It’s okay to feel frustrated or overwhelmed at times. Reach out for support when needed, whether from a mental health professional, a support group, or your loved ones.
Dermatitis Herpetiformis may change how you live, but it doesn’t have to define you. With knowledge, support, and resilience, you can navigate this new normal and live a fulfilling life.
Dermatitis Herpetiformis in Different Demographics: An Inclusive Look
Dermatitis Herpetiformis (DH), a skin manifestation of gluten sensitivity, is indiscriminate. It can appear at any age, showing no preference for your calendar age or life stage. However, some patterns are worth noting. According to available data, DH most often makes its initial appearance in those aged 15 to 40. These years, often filled with exploring new foods and environments, can suddenly become a battlefield as the body reacts to gluten dramatically and uncomfortably.
Facing Dermatitis Herpetiformis: A Journey, Not a Destination
The pathway with Dermatitis Herpetiformis may seem daunting, but I assure you, it’s manageable. My work in the field of immunology has shown me that we are making strides in understanding and managing this condition.
For those living with DH, the key is to remember that this is a journey, not a destination. It’s about finding what works for you regarding diet, symptom management, and emotional well-being. It’s about adapting to a new normal and resilience in a chronic condition.
Most importantly, it’s about not losing sight that you are more than your diagnosis. Dermatitis Herpetiformis may be a part of your life, but it doesn’t define you. A community of healthcare professionals, researchers, and fellow patients is here to support you at every step of your journey.
As research progresses, I’m confident we will see new developments and advances that will further improve the quality of life for those with DH. Until then, remember that you are not alone, and there is always hope.
Frequently Asked Questions About Dermatitis Herpetiformis
As a healthcare professional, I encounter numerous questions about Dermatitis Herpetiformis. I’ve compiled and answered some of the most frequently asked questions to help demystify this complex condition.
What triggers a flare-up of Dermatitis Herpetiformis?
Flare-ups of Dermatitis Herpetiformis are primarily triggered by ingesting gluten. Even small amounts can lead to a reaction. Other factors like stress or skin trauma may also contribute to flare-ups.
Can Dermatitis Herpetiformis go away on its own?
Dermatitis Herpetiformis is a chronic condition that doesn’t go away alone. However, strict adherence to a gluten-free diet can help manage symptoms and prevent flare-ups.
Is Dermatitis Herpetiformis contagious?
No, Dermatitis Herpetiformis is an autoimmune condition and is not contagious. It cannot be passed from person to person through skin contact or any other means.
Can children get Dermatitis Herpetiformis?
While Dermatitis Herpetiformis is more commonly diagnosed in adults, children can also develop this condition. The symptoms may differ slightly in children, and a gluten-free diet is equally important for managing the condition.
Can Dermatitis Herpetiformis be cured?
As of now, there is no cure for Dermatitis Herpetiformis. However, a strict gluten-free diet can effectively manage symptoms, and research is ongoing to find more effective treatments or even a potential cure.
References
- Antiga, E., Caproni, M., & Bonciani, D. (2012). The diagnosis and treatment of dermatitis herpetiformis. Clinical, Cosmetic and Investigational Dermatology, 5, 67–73. doi:10.2147/CCID.S25260.
- Zone, J. J. (2005). Skin manifestations of celiac disease. Gastroenterology, 128(4), S87-S91. doi:10.1053/j.gastro.2005.02.027.
- Salmi, T. T., Hervonen, K., Kautiainen, H., Collin, P., & Reunala, T. (2011). Prevalence and incidence of dermatitis herpetiformis: a 40-year prospective study from Finland. British Journal of Dermatology, 165(2), 354-359. doi:10.1111/j.1365-2133.2011.10385.x.
- Hall, R. P., 3rd, & Streilein, R. D. (2020). Dermatitis Herpetiformis. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- Mansikka, E., Hervonen, K., Salmi, T. T., Kautiainen, H., Kaukinen, K., Collin, P., & Reunala, T. (2018). The decreasing prevalence of severe villous atrophy in Dermatitis Herpetiformis: a 45-year experience in 393 patients. Journal of Clinical Gastroenterology, 52(2), 101-104. doi:10.1097/MCG.0000000000000862.
Disclaimer: This article is intended for informational purposes only. The content within does not serve as a substitute for professional medical advice, diagnosis, or treatment. Always seek advice from a qualified healthcare provider with any questions regarding a medical condition or treatment.”
This disclaimer emphasizes that the article’s content is meant to inform rather than serve as medical advice, encouraging readers to consult with a healthcare professional for their medical concerns.