Welcome to the intriguing world of dermatology! Today, we’re going to explore the phenomenon of Dermatofibromas. You might be wondering, ‘What is Dermatofibromas?’ It’s not a term you hear daily, but it’s a consistent part of their skin story for some. Dermatofibromas are small, benign, non-cancerous bumps that can appear anywhere on your skin. Although they are most commonly found on the arms and legs, these hard, raised growths can be as varied as the individuals they appear on, ranging in color from pink to brown or even purplish. They are also known for their unique ‘dimple sign.’ Intriguing, right? Let’s discover more about Dermatofibromas, their causes, symptoms, diagnosis, and the various treatment options.

What are Dermatofibromas?
Dermatofibromas, in the simplest of terms, are harmless skin growths. But there’s more to them than meets the eye. They result from an overgrowth of the skin’s connective tissue cells. Dermatologists believe they could be reactive, potentially triggered by minor injuries such as insect bites or thorn pricks. These little blemishes are like the skin’s way of remembering a past insult.
Visually, Dermatofibromas are firm, raised bumps, typically less than half an inch in diameter. However, don’t be surprised if you come across some that are larger. Their color can vary from person to person, some appearing pink, others brown, and a few with a purplish hue.
Let’s discuss their unique feature – the ‘dimple sign.’ When you pinch a Dermatofibroma, it dimples inward instead of popping out like most bumps. It’s an interesting attribute, isn’t it? This is due to how Dermatofibromas grow, embedding themselves deeper into the skin’s layers.
The Science Behind Dermatofibromas
A. Causes of Dermatofibromas
Here’s a puzzler: What causes dermatofibromas? The truth is, even with all our scientific advancements, the exact cause remains elusive. Researchers and clinicians have proposed several theories, though. Some believe minor skin injuries or insect bites might trigger their development. Others suggest they could be an immune response. Yet, no single theory has been universally accepted, making dermatofibromas all the more mysterious.
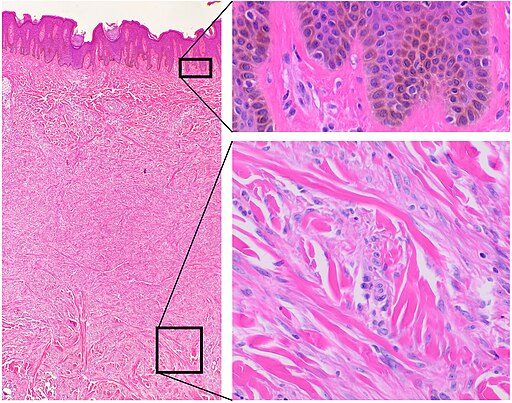
B. Understanding the Pathology
Dermatofibromas are essentially an overgrowth of the skin’s connective tissue. Picture this: your skin’s cells decide to hold a meeting, and too many show up, creating a visible bump. This simplistic view helps us grasp the essence of dermatofibromas, but the actual pathology is complex. It involves intricate cellular interactions and biological processes. But the bottom line is, despite their peculiar nature, dermatofibromas are benign and typically harmless.
Symptoms and Identification of Dermatofibromas
A. Common Symptoms
Dermatofibromas has a classic presentation: they appear firm and round, with raised bumps on the skin. However, they also have a few tricks up their sleeve. They may vary in color, from pink to brown or even purplish. Some might feel tender or itchy, especially when pinched. But the hallmark characteristic is the ‘dimple sign.’ When you pinch a dermatofibroma, it ‘dimples,’ diving deeper into the skin. This unique sign can help distinguish dermatofibromas from other skin conditions.
B. Identification and Diagnosis
Identifying Dermatofibromas might seem like a daunting task, especially considering how they can mimic other skin conditions. But don’t worry; we’ve got you covered. The key lies in understanding their unique characteristics and, of course, consulting with a dermatologist.
While the ‘dimple sign’ can be a good indicator, Dermatofibromas can feel tender or itchy, especially when pinched or rubbed. However, remember that self-diagnosis can be risky. Skin conditions can be deceptive, and what appears to be a simple Dermatofibroma could be a different skin issue altogether.
Therefore, if you suspect you have a Dermatofibroma, it’s best to schedule a visit with your dermatologist. They can provide a definitive diagnosis, often through a physical examination and, if needed, a skin biopsy. A skin biopsy involves taking a small skin sample for laboratory testing, allowing for an accurate diagnosis.
Treatment Options for Dermatofibromas
Dermatofibromas are benign, meaning they don’t risk your health. However, if they are causing discomfort or if you’re concerned about their appearance, there are several treatment options available.
One common approach is to leave them alone. Yes, you heard that right! Dermatofibromas usually don’t require treatment unless they become painful or itchy or if they’re causing you distress because of how they look.
Surgical removal is often the first line of action if treatment is needed. This procedure involves numbing the area around the Dermatofibroma and then using a scalpel to cut it out. While this method is typically effective, it can leave a scar.
Another treatment option is cryotherapy, which involves freezing the Dermatofibroma with liquid nitrogen. This procedure can help reduce the size and appearance of the growth, but it may not completely remove it.
Laser treatment can also be an option, especially for those concerned about potential scarring. Lasers can target and remove the growth with less damage to the surrounding skin.
Remember, the treatment choice largely depends on your personal preferences and the advice of your dermatologist. It’s essential to discuss these options thoroughly with your healthcare provider before deciding on a course of action.
Living with Dermatofibromas: Lifestyle and Management Tips
Living with Dermatofibromas can be a unique experience for each individual. For some, these growths may just be a slight cosmetic concern. In contrast, they can cause significant discomfort for others, especially if they are located in areas that frequently rub against clothing or are touched often.
Understanding that Dermatofibromas are benign and non-cancerous can help alleviate some of the worries associated with these skin growths. They don’t spread or turn into cancer, and they don’t affect your overall health.
However, if Dermatofibromas are causing discomfort or distress, it’s important to remember that you have options. There are multiple ways to address the issue, from surgical removal to cryotherapy and laser treatments. Most importantly, regular check-ups with your dermatologist can help manage any changes in your Dermatofibromas and update you on the latest treatment options.
Remember, everyone’s skin journey is different. What works for one person might not work for another. Therefore, finding a treatment plan that fits your needs and lifestyle is essential.
Dispelling Dermatofibroma Myths
Let’s face it, the internet can be a breeding ground for misinformation, and when it comes to medical conditions like Dermatofibromas, the myths can easily outweigh the facts. That’s why we’re here to set the record straight and dispel some common Dermatofibroma myths.
Myth 1: Dermatofibromas are contagious.
Truth: Absolutely not! Dermatofibromas are not contagious. They can’t be passed from person to person through touch or any other means for that matter. These skin growths occur as a response to minor injuries or insect bites. They are in no way a result of an infectious agent.
Myth 2: Dermatofibromas can turn into cancer.
Truth: Dermatofibromas are benign skin growths. They do not have the potential to become cancerous. While it’s always important to monitor any changes in your skin and consult a dermatologist if something seems off, Dermatofibromas should not cause cancer-related worry.
Myth 3: If you have one Dermatofibroma, you’ll get more.
Truth: Not necessarily. While some might develop more than one Dermatofibroma, it’s not a given. Each Dermatofibroma develops in response to a specific trigger, like an insect bite or minor skin injury.
Dispelling these myths is crucial in understanding Dermatofibromas and managing them effectively. Always seek reliable sources for your information and consult a dermatologist for any skin-related concerns.
A Closer Look at Dermatofibroma Removal Procedures
When dealing with dermatofibromas, one might consider removal procedures if they’re causing discomfort or their appearance is a concern. Let’s look at the three primary methods: surgical removal, cryotherapy, and laser treatment.
Surgical Removal
Surgical removal of dermatofibromas is typically an outpatient procedure performed under local anesthesia. The dermatologist uses a scalpel to excise the growth, and stitches may be required depending on the incision size. After the procedure, keeping the area clean and following your doctor’s advice to avoid infection and aid healing is essential. While this method is usually effective, it can leave a scar that concerns some individuals.
Cryotherapy
Cryotherapy is a less invasive method that involves the use of liquid nitrogen to freeze the Dermatofibroma. The extreme cold destroys the cells within the growth, causing it to gradually shrink over time. This procedure may cause some discomfort, but it’s often bearable. Possible side effects include skin discoloration and a small risk of nerve damage.
Laser Treatment
Laser treatment is a modern approach that uses focused light to heat and destroy the Dermatofibroma. It’s a precise method that causes minimal damage to the surrounding skin, reducing the risk of scarring. However, multiple sessions may be required depending on the size of the Dermatofibroma.
Remember, the best treatment option depends on individual circumstances, including the size and location of the Dermatofibroma, personal preferences, and overall health. Always discuss these factors with your dermatologist before making a decision.
The Psychological Impact of Dermatofibromas
While dermatofibromas are physically harmless, they can sometimes have psychological implications, particularly if they’re located in visible areas. Dealing with visible skin conditions can affect self-esteem and lead to feelings of self-consciousness. It’s not unusual for individuals with dermatofibromas to feel uncomfortable with their appearance, leading to decreased confidence and social interactions.
It’s important to remember that seeking help is okay if you’re feeling this way. Speaking to a mental health professional can provide strategies for coping with these feelings. Support groups, both online and in-person, can also offer comfort and understanding to people who are going through similar experiences.
Ultimately, remember that everyone’s skin tells a story; these unique aspects make us who we are.
Latest Research and Advances in Dermatofibroma Treatment
The field of dermatology is always evolving, with new research and advances continually emerging. In dermatofibromas, scientists explore the genetic and molecular mechanisms that lead to their formation. Understanding these pathways could open the door to new prevention strategies and treatments.
Currently, researchers are studying the efficacy of various laser treatments for dermatofibromas. Some studies suggest that specific types of lasers can be more effective at reducing the size and appearance of these growths with minimal scarring and recovery time.
While these advances are promising, they’re still in the research phase, and more studies are needed before they become standard treatments. However, they represent the exciting potential of what lies ahead in dermatofibroma treatment.
Unraveling Dermatofibromas: Final Thoughts
Dermatofibromas might be a mystery in many ways. Still, one thing is clear: they’re typically harmless skin guests that don’t overstay their welcome. Living with dermatofibromas can be a breeze with the right knowledge and management.
Frequently Asked Questions about Dermatofibromas
Let’s now address some frequently asked questions about dermatofibromas, providing comprehensive answers to satisfy your curiosity and concerns.
1. What exactly is a dermatofibroma?
A dermatofibroma is a common type of benign skin growth or lesion that often appears following minor injuries or insect bites. They are typically firm and raised and can vary in color from pink to brown.
2. How can I recognize a dermatofibroma?
Dermatofibromas are usually less than half an inch in diameter, feel firm to the touch, and may appear pink, brown, or purplish. They often develop on the legs but can appear anywhere on the body.
3. Are dermatofibromas dangerous?
No, dermatofibromas are benign, meaning they are not cancerous and do not pose a risk to your health.
4. Do dermatofibromas go away on their own?
Dermatofibromas are generally persistent and do not disappear without treatment. However, they do not pose a health risk and often do not require treatment unless they cause discomfort.
5. Can dermatofibromas be prevented?
Since the exact cause of dermatofibromas has yet to be fully understood, specific prevention strategies are challenging to provide. However, maintaining good skin health and promptly treating skin injuries or insect bites may help.
6. How are dermatofibromas treated?
If a dermatofibroma needs to be treated, methods include surgical removal, cryotherapy, or laser treatment. The best treatment depends on the individual’s preferences, the Dermatofibroma’s size and location, and overall health.
7. Does removing a dermatofibroma leave a scar?
Surgical removal of a dermatofibroma may leave a scar. Other methods, like cryotherapy and laser treatment, may result in less noticeable scarring.
8. Can a dermatofibroma turn into cancer?
No, a dermatofibroma is a benign skin growth and does not have the potential to turn into cancer.
9. Are dermatofibromas contagious?
No, dermatofibromas are not contagious. They cannot be passed from person to person.
10. What’s the latest research on dermatofibromas?
The field of dermatology is continually evolving, with research currently focused on the genetic and molecular mechanisms that lead to dermatofibroma formation. Advances are also being made in laser treatments, with promising results in reducing the size and appearance of dermatofibromas.
References
- Alves JVP, Matos DM, et al. Variants of Dermatofibroma – a histopathological study. An Bras Dermatol. 2014 May-Jun; 89(3): 472–477. Accessed 4/8/2022. Available at NCBI.
- Johnson, Jon. Dermatofibroma: Causes, images, and treatment. Medical News Today. Updated on August 31, 2021. Available at Medical News Today.
- Oakley, Amanda. Dermatofibroma. DermNet NZ. Revised September 2020. Available at DermNet NZ.
Disclaimer: This article is intended for informational purposes only. The content is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read in this article. The references used in this article do not cover all possible information, drugs, instructions, or tests that could be relevant to your health.