A Definitive Guide to Porokeratosis: The Different Types, Causes and Treatment Options
Even though Porokeratosis is a rare condition, it is known to affect people of all ages. This skin disorder was discovered in 1893 by two Italian physicians, Mibelli and Respighi. Since 1893, thousands of people have been reported to have had Porokeratosis. If you suspect that you or a loved one may have Porokeratosis, this article will explain more about this condition, including the symptoms and the best treatment options.
What is Porokeratosis?
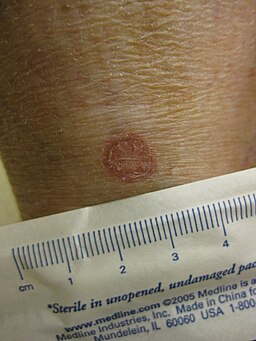
It’s a skin disorder where tiny round patches develop on your skin. These patches have a thin, raised edge. Porokeratosis is divided into several sub-categories. Each type has unique symptoms, which we will discuss in detail later.
In most scenarios, this skin disorder isn’t a cause for alarm. Nonetheless, some Porokeratosis cells can be cancerous. That’s why seeking a professional medical diagnosis is advisable to rule out any risks.
Patches on the skin caused by Porokeratosis can be brown, red, or Pink. Depending on the Porokeratosis subtype, these patches can appear on one body part or in different areas. Despite being a skin disorder, Porokeratosis is not contagious. Therefore, you can’t spread it to another person, nor can you spread it to another part of your body.
The 6 Different Types of Porokeratosis
To understand what Porokeratosis is and how best to treat it, you should familiarize yourself with the different subtypes. That’s the easiest way to diagnose the disorder affecting you or a loved one.
1. Disseminated Superficial Actinic Porokeratosis
Abbreviated as DSAP, this is the most popular type of Porokeratosis, and it’s prevalent in younger and middle-aged adults in their 20s to 40s. Research also shows that it affects more women than men.
DSAP mostly appears as brown or red scaly rings on the shoulder, legs, arms, and back. These spots can also be itchy. Scientists believe that DSAP can be genetically inherited or caused by UV light exposure. Radiation therapy is also a possible trigger for DSAP.
2. Mibelli Porokeratosis
This subtype was named after one of the Italian doctors who discovered this condition. It’s also the second most popular type of this skin disorder. The Mibelli version is more prevalent in men than women. And it affects mainly children and young adults.
Mibelli Porokeratosis manifests itself as tiny brownish bumps. Therefore, they are easier to see or diagnose. This subtype mainly occurs on the limb but can appear anywhere in the body.
Various factors, such as extensive use of topical steroids, exposure to radiation, and light therapy, can cause it. However, rarely does Mibelli Porokeratosis develop into cancer.
3. Punctate Porokeratosis
Punctate Porokeratosis is easy to diagnose because the bumps formed resemble seeds and only appeared on soles and palms. It is a rare version of Porokeratosis. Therefore, to determine which gender is at higher risk or what are the potential triggers there is not enough research. But we do know that it mainly affects developing adults. Secondly, you have a higher chance of getting Punctuate Porokeratosis if you have any of the above types. Patients with Punctate Porokeratosis repost discomfort or itchiness when walking.
4. Linear Porokeratosis
It’s another rare Porokeratosis that affects the soles and palms. But in this version, the lesions are reddish-brown and appear uniformly. Linear Porokeratosis affects mostly women and occurs during the early stages of childhood.
5. Porokeratosis Palmaris et Plantaris Disseminata
This subtype is mainly referred to as PPPD and is less common than the first two. PPPD affects more men than women. It develops younger adults, especially those transitioning from their teenage years. In this subtype, lesions appear uniformly, resembling your skin color, and may not have a border. However, with PPPD, the patches might have tiny yellow pits. PPPD mainly occurs on the soles and palms.
6. Disseminated Superficial Porokeratosis
If you have noticed round brown bumps on a child aged five to ten, there is a high chance that it is Disseminated Superficial Porokeratosis. This subtype can appear on any part of the body. But the distinguishing factor is that the lesions appear on a wide skin area. Unfortunately, we don’t know much about the triggers and whether the cells are cancerous because this skin condition is rare.
How to Diagnose Porokeratosis?
A certified doctor or dermatologist should make the diagnosis of Porokeratosis. First, they will perform a physical examination of the lesions. Then, they may use methods such as dermatoscopy or a biopsy. The latter aims to determine whether cancerous cells are present on the bumps.
However, a physical analysis of the scalpy patch can contribute significantly to helping the doctor identify Porokeratosis. The patch’s location is another crucial contributor because DSAP and PM occur on the arms and legs, whereas Mibelli Porokeratosis can appear anywhere.
During diagnosis, it’s essential to be open with your dermatologist. You should disclose whether the lesions are appearing on your genitals. It’s also crucial to mention other symptoms you may be experiencing, such as itchiness or discomfort.
What are the Main Causes?
Even though Porokeratosis was discovered more than a century ago, the causes of many subtypes remain unknown because the condition is rare. However, existing research has identified some of the following triggers.
- UVExposure: Some subtypes of Porokeratosis, such as DSAP, are known to be caused by exposure to sunlight.
- Genetics: You can inherit Porokeratosis cells from either the father or mother.
- A Weak Immune System: People living with conditions that contribute to a suppressed immunity can develop Porokeratosis.
- Excessive Usage of Topical Steroids: Some topical corticosteroids are known to worsen skin infections. If Porokeratosis is dormant in your skin, these topical steroids can trigger it.
- Additional causes of Porokeratosis include radiation therapy and burns.
Who is at Risk of Getting Porokeratosis?
When listing the different subtypes of this skin disorder, we mentioned that some people are at a higher risk of being affected. Some of the factors that put you at a higher risk include the following;
- Age: Some subtypes of Porokeratosis, like Disseminated Superficial Porokeratosis and Linear Porokeratosis, affect kinds, whereas Punctuate Porokeratosis and DSAP affect adults.
- Gender: Similar to age, some versions of Porokeratosis mainly affect more women than men and vice versa.
- Genes: If a parent or grandparent had Porokeratosis, you are at a higher risk of developing the same condition due to inherited genes.
- Skin color: People with fair skin are also at a higher risk of getting Porokeratosis.
Treatment
Unfortunately, no treatment can fully cure Porokeratosis. But the good news is that certain medications and procedures can ease the symptoms and appearance of these lesions. You and your doctor can explore these options and find the one that best addresses your condition.
- Imiquimod Cream: This cream is mainly used to treat warts but can also be used on Porokeratosis, especially the Mibelli subtype. Imiquimod creams trigger the immune system to eradicate abnormal skin growths such as Porokeratosis lesions. This is the most common treatment for this skin condition.
- Topical Vitamin D: Research shows that continued use of Topical Vitamin D can heal some versions of this skin disorder.
- Systemic Retinoids: Subtypes of Porokeratosis, such as Mibelli, respond well to topical retinoids
- Skin Procedures: In severe scenarios of Porokeratosis, your dermatologist may recommend invasive procedures such as laser therapy, cryotherapy, or dermabrasion to remove the lesions.
Regarding the treatment for Porokeratosis, you and your doctor need to find a suitable long-term solution. Whether you settle for topical ointments or therapeutic procedures, you must find a treatment plan that works best.
To find the best treatment solution, you need to consider the subtype of Porokeratosis you are dealing with. However, this is something you can handle.
It’s crucial to seek treatment for this skin disorder because the lesions can grow larger or spread to other parts of your body. Also, there is a risk of the cells becoming cancerous. The earlier you identify and start treating Porokeratosis, the more control you will have over this condition.
Home Remedies for Porokeratosis
A few homemade Porokeratosis remedies can help with the itching and discomfort, including Vitamin D and E oils. Lavender Oil can also offer some therapeutic benefits. In addition, some reports say apple cider vinegar can help eliminate Porokeratosis lesions. But we would advise you to stick to doctor-approved creams and ointments.
Part of Porokeratosis home care entails limiting exposure of the lesions to sunlight. When outdoors, you should cover the patches. It’s also good practice to put on sunscreen. As mentioned earlier, UV light can trigger or worsen this skin disorder.
It would be best if you also kept a close eye on Porokeratosis lesions. In case the patches start to grow bigger or change color, you should contact your doctor immediately. Don’t hesitate to do the same if you suddenly experience acute pain, discomfort, or bleeding.
How to Differentiate Between Porokeratosis and Ringworm?
Since Porokeratosis is rare, most people confuse it with a ringworm skin infection.
There are a couple of notable differences between a ringworm infection and Porokeratosis. First, a ringworm infection looks a bit different. The raised ring is often red with rashes; at the center, the skin color remains the same or turns pale. As for Porokeratosis, the lesion has a uniform color from the edges to the center.
Another obvious difference is that ringworm infections are contagious. People can transfer ringworm infections to other people and parts of the skin. Porokeratosis is not contagious. A ringworm infection is often caused by fungus and can be treated using an OTC anti-fungal cream. That’s not the case with Porokeratosis.
If you are having trouble distinguishing between Porokeratosis and a ringworm infection, your doctor or dermatologist can provide you with an accurate diagnosis or treatment plan.
Before we move on to the next topic, you must also differentiate Porokeratosis from warts and calluses. This will help you avoid wasting money and time treating the wrong type of lesion.
Does Porokeratosis Commonly Affect the Feet?
In the past few years, there have been several reports about foot Porokeratosis. Those affected narrate that lesions appear on the bottom of their feet, making walking uncomfortable.
When listing the different subtypes of Porokeratosis, we mentioned some, such as the Punctate, which affects the soles. This most common subtype can develop anywhere on the bottom of your feet, making walking pretty painful.
Foot Porokeratosis, like other versions, it’s not treatable, but you can manage it. The best solution is to have the lesions carefully removed by a podiatrist or dermatologist. This usually brings therapeutic relief to the patient.
Sometimes, these lesions can grow back. In such a scenario, your dermatologist can recommend cryotherapy because it prevents the lesions from growing back for much longer. In addition, you can use various prescription creams to treat and care for Porokeratosis developing on the feet.
Some studies have also shown that clogged sweat glands can cause Porokeratosis on the feet. However, research is still underway. In such a scenario, your doctor can recommend treatment using creams or lesion removal techniques. In addition, it’s crucial to control feet sweat by switching to breathable shoes or socks and using foot antiperspirants or powders.
To Wrap Things Up
Six main types of Porokeratosis appear on different parts of the body. You should consult your doctor for a professional diagnosis if you suspect this skin disorder. A licensed dermatologist can identify which subtype of Porokeratosis that’s affecting you. They can also recommend one or two of the treatment plans listed above.
Even though there is no cure for Porokeratosis, it is manageable, and with the right treatment plan, you can ease the symptoms and appearance of these scaly patches. It’s, however, important to frequently observe and take care of these lesions.